During World War II, it was discovered that many survivors of shipwrecks suffered from internal lung injuries caused by underwater explosions of depth charges; however, these injuries showed no external signs of trauma. This was the first evidence that shockwaves produced by explosions could cause serious damage to human tissue.
In the 1950s, researchers began to systematically study the medical potential of shockwaves. Early experiments revealed that electrohydraulic shockwaves were powerful enough to break ceramic plates submerged in water. In the United States, Frank Rieber from New York was granted the first patent for an electrohydraulic shockwave generator (Patent No: 2,559,277). By the end of the decade, the basic physical principles of electromagnetically generated shockwaves had also been documented. 5 16
Shockwave therapy (ESWT) was first developed in the 1980s to break up kidney stones and quickly became a major innovation in the medical world. 2,4,6 Focused acoustic waves produced outside the body reach the target area without damaging surrounding tissues, providing a therapeutic effect. This feature has transformed the method into a modern technology that can be applied without the need for surgery.
Over time, research has shown that shockwaves are not limited to breaking stones but also accelerate healing processes in bones, tendons, and soft tissues. 16,20
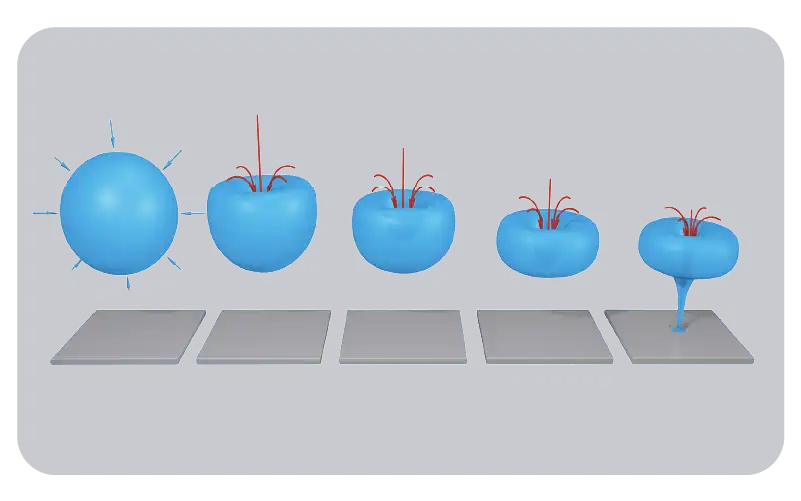
The effect of ESWT, begins with the transfer of the mechanical energy of the waves to the tissues, triggering a series of biological responses at the cellular level. It stimulates the formation of new blood vessels (angiogenesis), supports cell regeneration, and thus accelerates tissue repair. 11,12,18
It also relieves pain by reducing certain pain-transmitting substances in nerve endings (e.g., substance P, CGRP). 5
Today, ESWT is applied in two ways:
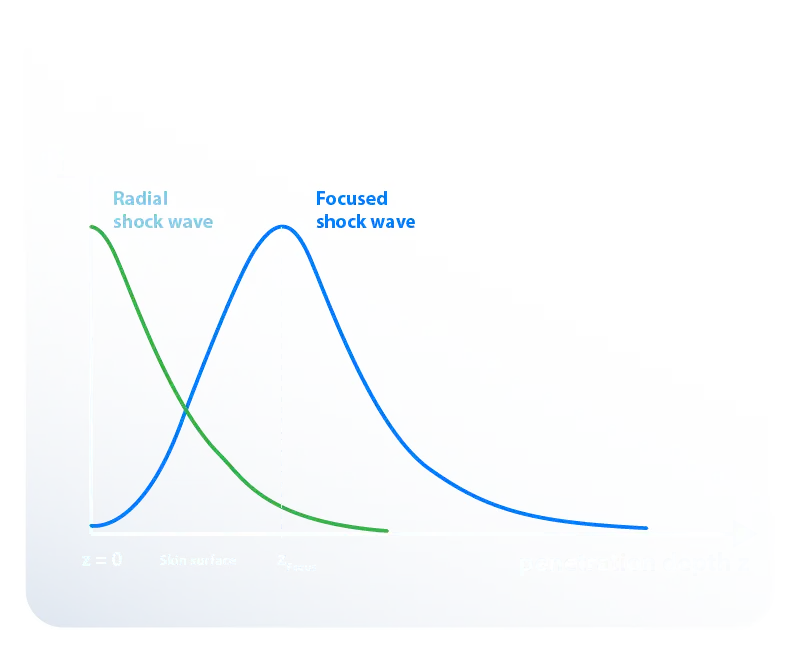
• Focused shockwaves (fESWT): Reaches deep tissues and creates powerful biological effects. It is particularly used in non-uniting fractures, chronic tendon diseases, Peyronie's disease, and erectile dysfunction. 10,13Research shows that focused shockwaves provide more lasting biological healing in the long term, while radial shockwaves offer faster symptomatic relief. 13
Focused shockwave generators are capable of creating true shockwaves at the focal point, while radial devices only produce pressure (acoustic) waves. 4 These waves can reach pressure levels of up to 30 MPa, but their rise times are quite slow; around 3 microseconds. 4
Today, ESWT is used as a safe and effective treatment method in many fields, from orthopedics to urology, from sports medicine to circulatory disorders. It also carries strong potential in the fields of vascular diseases and regenerative medicine. 1,7
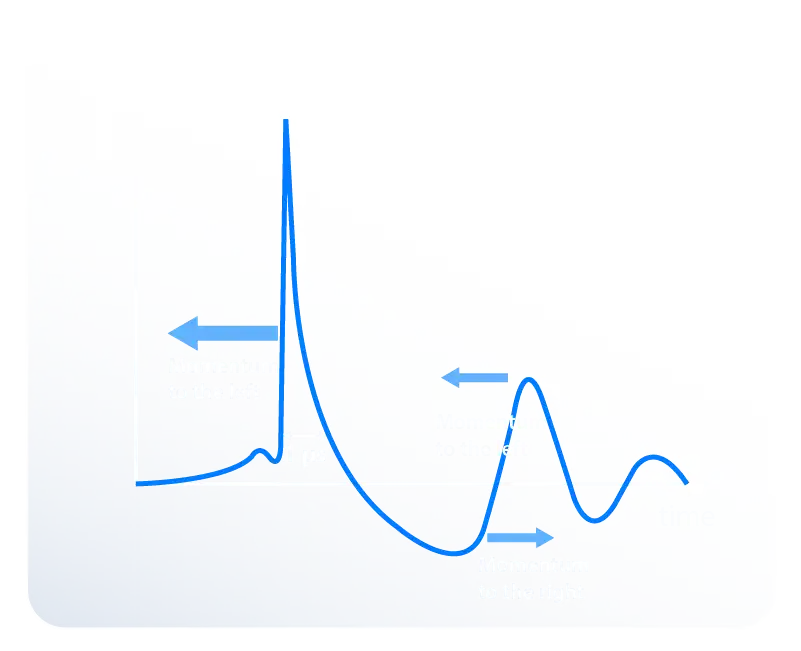
Focused shockwaves are short-duration, high-pressure acoustic waves. They are produced outside the body (extracorporeal) and focused on tissue. They contain a high positive pressure peak (P⁺) followed by a small negative pressure phase (P⁻). Thanks to this special structure, they penetrate deep into tissues, support tissue regeneration, and produce medical effects like stone fragmentation.
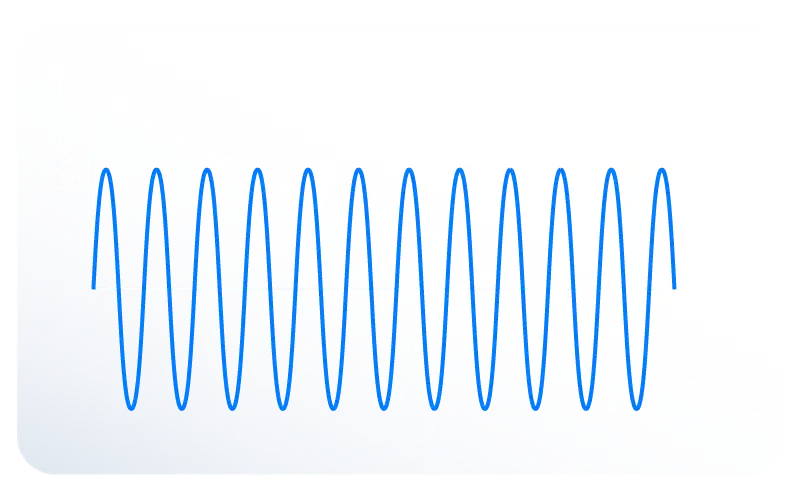
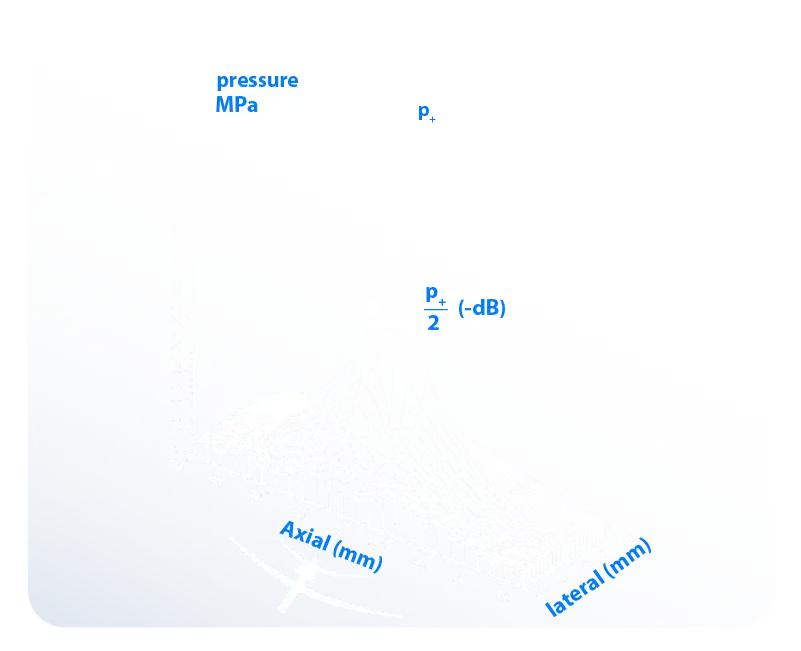
From a physical perspective, a shockwave is defined by a sudden and almost instantaneous pressure jump and propagates at a speed higher than the speed of sound in the medium it is in. 16 Fig. 1 shows a representative pressure profile of a therapeutic focused shockwave. A shockwave fundamentally consists of a single pulse that covers a very wide frequency spectrum (approximately 150 kHz to 100 MHz). This wave reaches extremely high pressure peaks (up to 150 MPa) followed by a tensile phase that can drop to –25 MPa.
Another feature that distinguishes shockwaves is their extremely short pulse duration and an exceptionally fast rise time lasting only a few hundred nanoseconds. 3
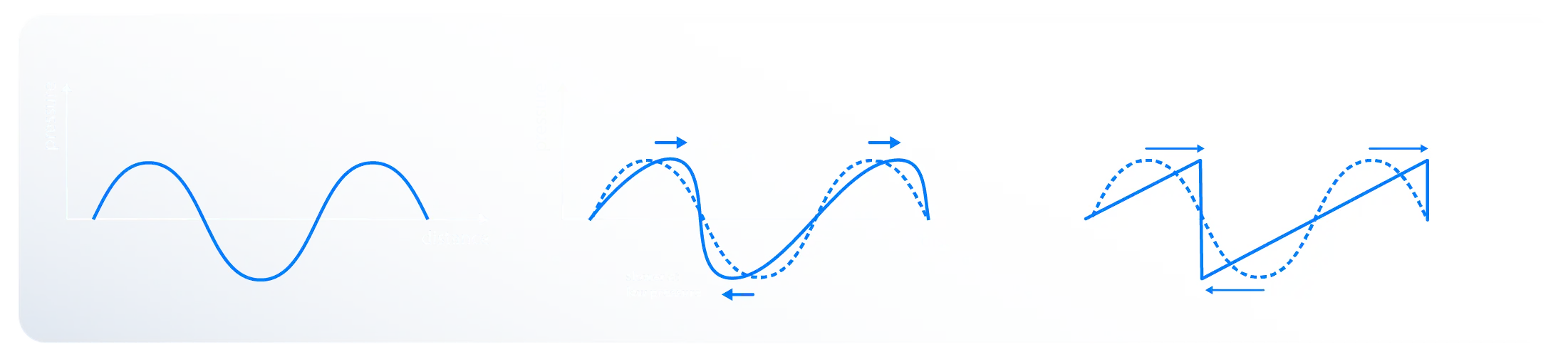
Both ultrasound and shockwaves are acoustic waves, but there are some fundamental differences. Ultrasound waves consist of narrowband, periodic oscillations and are mostly used for imaging and diagnostic purposes. In contrast, shockwaves consist of a single high-pressure peak and a short negative phase. They are broadband, high-pressure, and applied for therapeutic purposes.
They also differ in terms of propagation: ultrasound waves propagate linearly, while shockwaves propagate nonlinearly, a process that leads to wave steepening. 4,6

Focused shockwaves can be produced via electrohydraulic, piezoelectric, or electromagnetic generators. In electrohydraulic systems, shockwaves are generated directly from the source. In piezoelectric and electromagnetic systems, shockwaves are formed as a result of wave steepening and superposition effects. Therefore, the shockwave reaches its maximum intensity only in the focal region.4,6
The focal sizes of shockwaves produced by different generator types vary. The focus is smallest in piezoelectric systems, while the largest focal area is obtained in electrohydraulic systems. This indicates that the dose of the shockwave to be used in treatment depends on the type of generator selected. 9,16
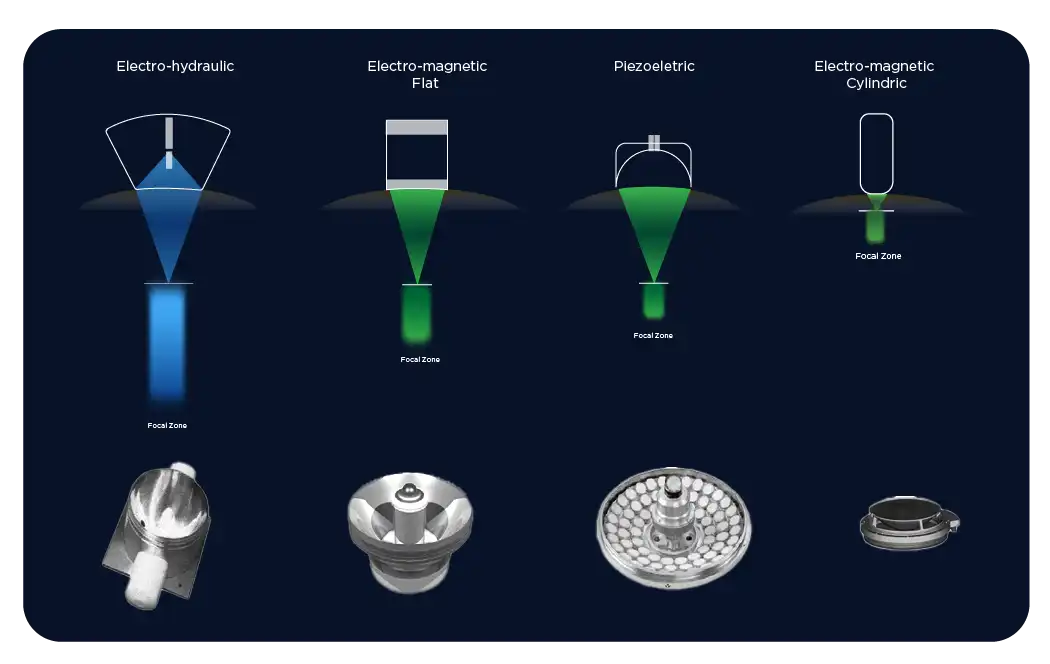
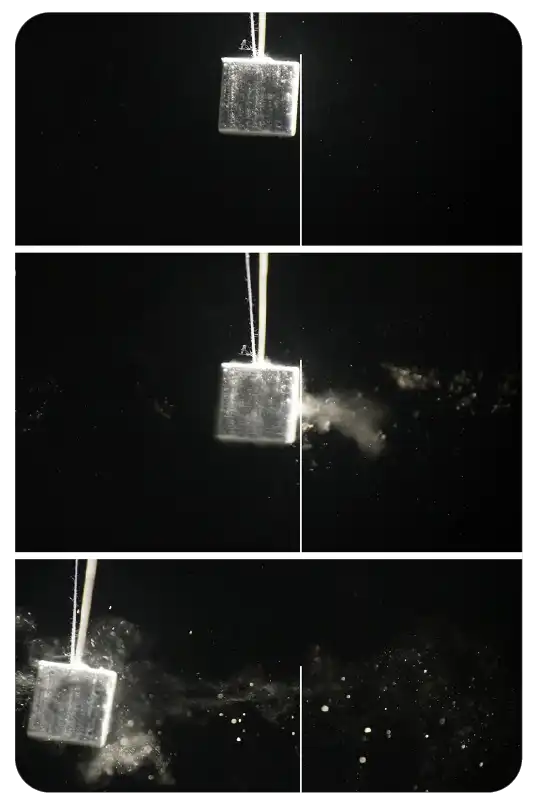
The electrohydraulic shockwave generation method is based on the spark discharge principle. A short-duration, high-voltage discharge occurs in the gap between a pair of electrodes, and this rapid energy release creates a plasma bubble in the surrounding fluid medium. A high-pressure acoustic wave is produced with the collapse of the plasma bubble. 4,6
The shockwaves obtained with this method are focused by parabolic reflectors and directed to the tissue. Electrohydraulic systems have been used safely for many years for breaking kidney stones (ESWL) and in orthopedic indications due to their strong focusing and wide energy range.9,16

Focused shockwaves are acoustic waves like sound waves and require a medium to propagate. This medium is usually a conductive material like water or gel. Since most human tissues consist of water, shockwaves travel through tissues with very little loss.
These transmission properties are explained by a physical concept called acoustic impedance (Z):
Z = ρc
(ρ = density, c = speed of sound)

The density and sound transmission speed of different tissues vary. Therefore, as shockwaves pass from one tissue to another, they can change direction, be reflected, or lose some of their energy. This can be thought of as being similar to how light refracts in different media like glass or water.
This effect is important from a therapeutic perspective: because the losses that occur at the interfaces must be minimized for energy to be transmitted correctly to the targeted tissue. For this purpose, special coupling systems have been developed in shockwave devices. While in the first devices the patient sat directly in a water-filled tub, modern systems now use a gel or a thin layer of water to eliminate the air gap between the device and the skin. In this way, energy loss is minimized, and the maximum effect is transmitted to the focal point.
Clinical Importance: If the acoustic impedance difference between two tissues is large (for example, between soft tissue and bone), a significant portion of the shockwaves may be reflected. Therefore, how the waves will travel within the body should be carefully evaluated during treatment planning.
In the transmission of focused shockwaves to the body, the absence of an air gap between the device and the skin is of critical importance. This is because air bubbles or gas-containing areas absorb or reflect a large portion of the energy, reducing the effectiveness of the treatment. Therefore, modern devices use coupling with gel or a thin layer of water and eliminate potential air gaps.
Note: Air bubbles trapped between the source and the tissue can severely reduce the effect of the shockwave.
Not only the skin and soft tissues, but also other structures in the body play a role in the transmission of shockwaves. Gas-filled organs (e.g., the lung) or dense bone tissues can block the passage of waves. Therefore, the presence of these areas in the focal field during treatment is considered a contraindication.16
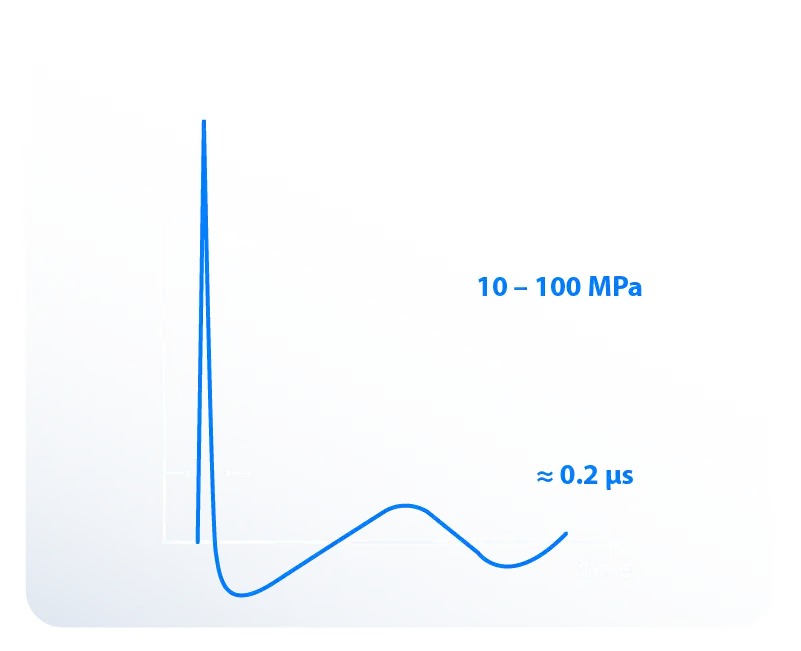
The characteristic properties of shockwaves are best measured using pressure sensors. Focused shockwaves used in medical applications typically reach peak pressure values (P⁺) between 10–100 MPa. This is equivalent to approximately 100 to 1000 times atmospheric pressure. 3,6
Depending on the shockwave formation mechanism, the rise times are extremely short (in the range of 10–100 nanoseconds). The pulse duration is about 1 microsecond (1000 nanoseconds), which is a fundamental feature that distinguishes shockwaves from classic medical pressure waves. 3
Another feature that distinguishes shockwaves is the presence of a smaller-amplitude negative pressure (P⁻) phase in addition to the high positive pressure peak (P⁺). The negative phase is typically about 10% of the P⁺ value and plays a critical role in the formation of the cavitation effect in tissues. 4
The P⁺ values measured in the focal region are modeled with three-dimensional pressure distribution graphs. This model is generally described with a pressure map in the shape of a mountain peak. There is a high-pressure peak point in the center, with gradually decreasing pressure values in the surrounding area. Therefore, the focal area of the shockwave is defined as the region where the pressure is greater than 50% of the maximum value (also known as the –6 dB focal region or the FWHM – full width at half maximum criterion). 5
Clinical Importance: Measurement parameters may vary depending on the type of shockwave generator used. The pressure profiles obtained from electrohydraulic, piezoelectric, or electromagnetic systems are different.
The most prominent effect of shockwaves occurs at the interfaces of different tissues or materials. The wave generally travels without loss within homogeneous tissues; however, pressure forces are released in regions with a difference in acoustic impedance. This is why shockwaves can pass through many tissues without causing harm, while creating a powerful destructive effect in hard structures (e.g., stone or bone), and biological stimulation in soft tissues. 11,18
Thanks to high-frequency components and short pulse structures on a millisecond scale, shockwaves can reach deep tissues and show a selective effect. In the process, cell membranes are stretched for a short time, permeability increases, and the mechanotransduction process begins. In this process, tissue regeneration is triggered by the release of nitric oxide (NO), growth factors, and other biochemical mediators. 11
As a result, shockwaves show both mechanical and biological effects at interfaces: 4
• In hard tissues → Fragmentation and breaking effect
• In soft tissues → Cellular stimulation and regenerative effect
Focused shockwaves provide concentrated energy transfer in a limited area, allowing the treatment to be directed to the target tissue. In this way, surrounding tissues are protected, while the therapeutic effect is created only on the affected area.
Clinical studies have shown that shockwaves in most cases increase blood circulation, accelerate metabolic activity and thus initiate the healing process. 11,12
The shear and pressure forces of shockwaves make cell membranes permeable for a short time. This mechanism is called mechanotransduction and is at the heart of many biological effects. 11
The main effects demonstrated by scientific evidence are:
• Increased cell membrane permeability
• Stimulation of microcirculation (blood and lymph flow)
• Release of Substance P
• Reduction in unmyelinated nerve fibers → pain modulation
• Release of nitric oxide (NO) → vasodilation, increased metabolism, angiogenesis, anti-inflammatory effect
• Antibacterial effect
• Release of growth factors and hormones (vessels, epithelium, bone, collagen)
• Stimulation of stem cells
• Neuronal stimulation (neuronal activity, neural spiking)
For Radial Pressure Waves (RPW) and/or Low-Energy Focused Shockwaves:
1.1. Malignant tumor in the treatment area (not as an underlying disease)
1.2. Fetus in the treatment area
Relative Contraindications
1.3. Epiphyseal plate in the treatment area
1.4. Brain or spine in the treatment area
Absolute Contraindications for High-Energy Focused Shockwaves:
1.5. Lung tissue in the treatment area
1.6. Malignant tumor in the treatment area (not as an underlying disease)
1.7. Severe coagulopathy
1.8. Fetus in the treatment area
Energy-Dependent Areas of Effect
The biological and mechanical effects created by shockwaves depend on the energy flux density (ED) used:
• Low-energy: Cellular regeneration, pain treatment, soft tissue healing
• Mid-energy: Pseudoarthrosis, chronic muscle-tendon pathologies
• High-energy: Stone fragmentation (lithotripsy) and fragmentation of hard tissues
Thus, the same technology can be used in both regenerative medicine and destructive applications. 4
The region where the biological effects of shockwaves occur is related not only to the size of the focal area but also to the absolute pressure values reached. Therefore, the 5 MPa threshold has been defined as the minimum pressure level at which a shockwave can be considered therapeutically effective.3,6
This approach is different from the –6 dB focal region of focused shockwaves. The –6 dB criterion defines the area that remains above 50% of the peak pressure. In contrast, the 5 MPa treatment zone refers to the area where the pressure value is equal to or higher than 5 MPa (approximately 50 bar). Therefore, the 5 MPa treatment zone is generally wider than the –6 dB focal region and varies depending on the energy level. 9,16
To date, there is no direct clinical study proving that the 5 MPa value is the definite biological effectiveness limit. However, experimental findings indicate that below a certain minimum pressure threshold, shockwaves show only limited or no therapeutic effect in tissue. 5
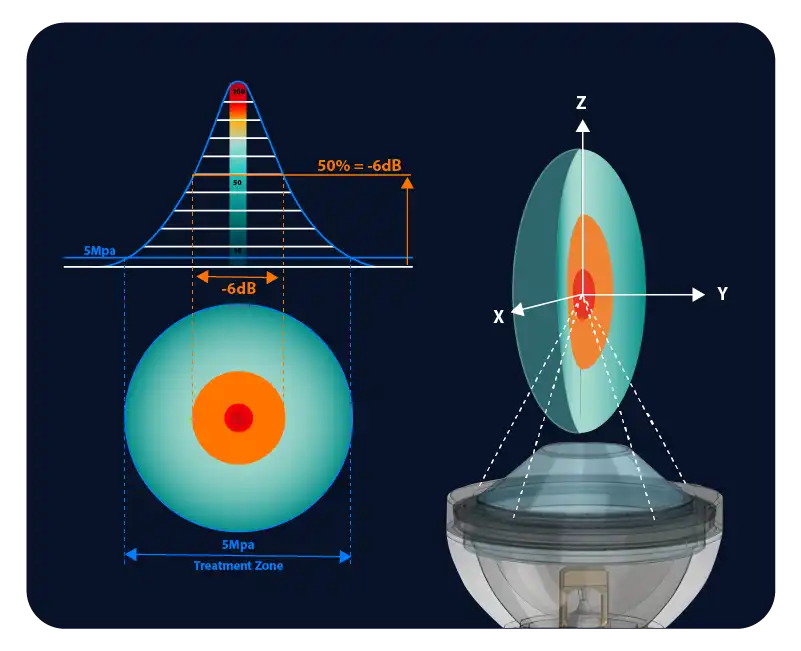
Clinical Importance: While the –6 dB focal region is a technical parameter of the device, the 5 MPa treatment zone better reflects clinical efficacy. This is because the biological response is directly related to the absolute pressure values.
Shockwave energy is one of the most fundamental parameters in medical applications. For a shockwave to have a therapeutic effect in tissue, certain energy thresholds must be exceeded 3,6.
Energy is calculated from the integral of the pressure-time curve. Mathematically, it is expressed as:
Here:
• A = area of the wave's effect
• Z = acoustic impedance
• p(t) = pressure function
The total energy (E_total) can be calculated by considering only the positive pressure phase (E₊) or by including the negative (tensile) phase as well. A shockwave pulse's energy is usually given in mJ (millijoules). Since hundreds or thousands of pulses are applied in clinical applications, the total energy is obtained by multiplying it by the number of pulses 5.
The effectiveness of treatment depends not only on the total energy but also on which area the energy is spread over. Therefore, “Energy Flux Density (ED)” is considered one of the most important parameters determining clinical efficacy. 16
Mathematically, ED is defined as:
The ED value is usually expressed in mJ/mm². This parameter shows the energy density of the shockwave and is used to classify the application as “low-intensity” or “high-intensity”. Low ED values are preferred for regenerative treatments (e.g., orthopedics, andrology), while high ED values are used in applications such as lithotripsy. 16.
Clinical Highlight: ED is the fundamental parameter that makes comparison between different devices possible. Looking at total energy alone is not enough; how the energy density is transferred to the tissue determines the clinical outcome.
A often-overlooked but very important property of shockwaves is that they carry momentum. As with energy, the momentum of a shockwave is defined by the integral of pressure over time. However, unlike energy, it is not necessary to square the pressure here; this preserves the sign of the pressure. As a result, the shockwave transmits a strong forward momentum with the positive pressure phase, and a smaller backward momentum with the negative tensile phase, 3,1
The asymmetric pulse structure of the shockwave makes these two momenta unable to cancel each other out, resulting in a net forward momentum. This is different from continuous ultrasound waves, where successive compression and tension phases largely cancel each other out, creating a negligible net momentum.
Shockwave momentum is critical in both high-energy lithotripsy (ESWL) applications and low-energy biological stimulation (ESWT) treatments. In ESWL, strong momentum creates a fragmentation force on hard tissues, while in ESWT, the lower-intensity momentum triggers biological stimulation and regeneration processes in soft tissues. 4
As the shockwave propagates in homogeneous tissues, momentum transfer is largely conserved. However, when the density (ρ) or speed of sound (c) of tissues changes suddenly — that is, when differences in acoustic impedance Z=ρcZ = ρcZ=ρc occur — a portion of the momentum is transmitted, while another portion is reflected. This ratio is expressed by the reflection coefficient: 6
At hard interfaces (e.g., stone, bone), a large part of the wave is reflected, while in soft tissues (e.g., muscle, tendon), most of the momentum is transmitted. This directly determines the clinical efficacy of shockwaves.
Another element related to momentum is force creation. According to Newton's law, every change in momentum must be accomplished by a force:
Therefore, when a shockwave reaches an interface, the change in momentum creates measurable forces. These forces can fragment structures prone to breaking (e.g., stones) or stimulate elastic tissues (e.g., muscle, connective tissue) to trigger biological responses⁵.
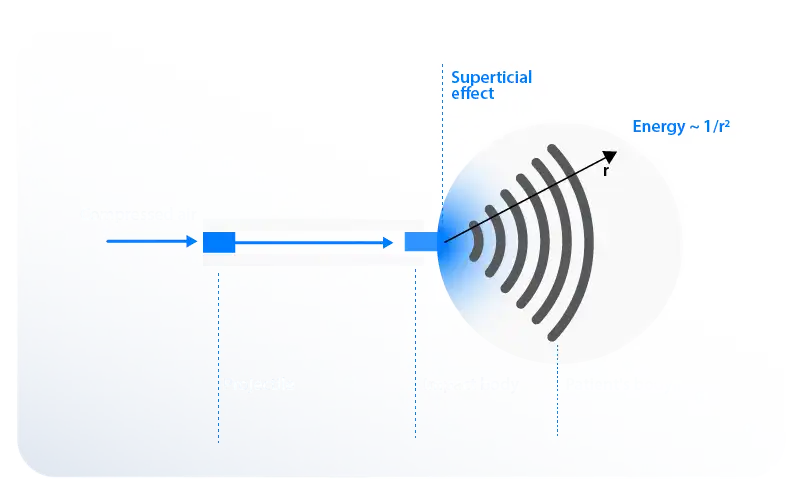
Radial Pressure Waves are obtained by converting mechanical energy into acoustic pressure waves via a ballistic system. Unlike focused shockwaves, these waves cannot be focused, have longer pulse lengths (0.15–1.5 m), and spread superficially. Therefore, from a physical standpoint, it is not a true “shockwave”; however, for ease of understanding in medical applications, it is often referred to as Radial Shockwave Therapy (RSWT). 19
Since the 1990s, radial pressure waves have become effective in the treatment of musculoskeletal disorders thanks to the mechanical energy transferred to the tissue. It supports pain control and healing in conditions such as tendinopathies, muscle injuries, and plantar fasciitis.20 The mechanism of action is based on Newton's law of action and reaction. 8
A significant clinical advantage is that it offers a lower-cost alternative compared to focused shockwaves. Research shows that the treatment outcomes obtained with radial pressure waves are similar to those with focused shockwaves in many indications.17 With these features, it is widely used as a reliable, effective, and economical treatment option in modern medicine.

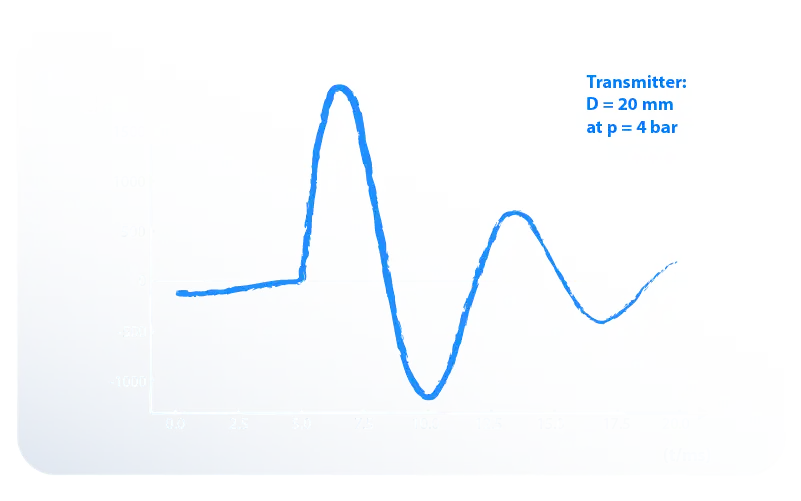
Radial pressure waves are produced by a ballistic mechanism where a projectile accelerated by a impact body (a moving object) strikes an impact body. The projectile, which is generally accelerated by compressed air, moves at a speed of approximately 5–25 m/s and decelerates abruptly upon impact with the impact body. A portion of the kinetic energy that arises during the collision is transferred to the impact body. 19
The impact body is the head part that directly contacts the patient's skin during treatment. This body moves back and forth a very short distance (usually <1 mm) at a low speed after the collision, transmitting the energy to the tissue.19 When energy is transferred in this way, the wave propagates in the tissue in a circular (radial) manner from the surface outwards.8
• Pressure level: The peak pressures of radial pressure waves are between 0.1–1 MPa. This value is significantly lower than that of focused shockwaves (10–100 MPa). 17
• Pulse duration: The pulse duration of radial pressure waves is approximately 0.2–5 ms. This duration is about 1000 times longer than that of focused shockwaves.20
• Energy propagation: Energy is concentrated in superficial areas from the point of contact; its effect on deep tissues is limited. 8
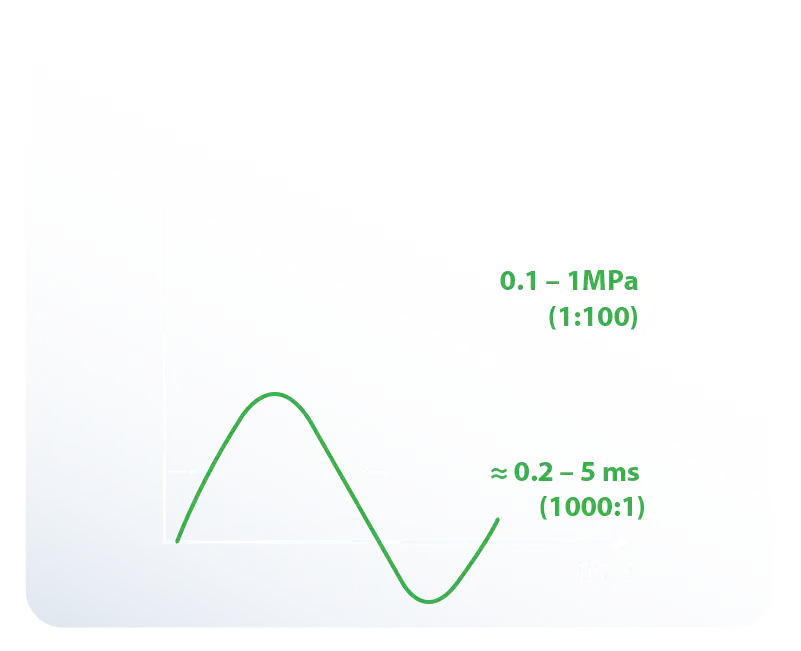
Due to these physical properties, radial pressure waves are preferred for superficial tissue treatments compared to focused shockwaves.
• Indications: Musculoskeletal disorders (tendinitis, muscle spasms, myofascial pain syndrome, etc.)
• Advantages: Simpler device structure, lower cost, wide range of clinical applications. 19, 17
Radial pressure waves propagate radially from the impact body's application point into the surrounding tissues. The energy density decreases rapidly with distance from the source (showing a drop of approximately 1/r²). Therefore, the strongest effect occurs on the skin surface or in the areas closest to the surface. The depth of the therapeutic effect is usually limited to 3–4 cm, but it reaches its highest intensity on the surface. 19
The pulse duration of radial pressure waves is much longer than that of focused shockwaves, and the pressure amplitude is lower. Therefore, classical water tank measurements used for shockwaves do not provide accurate results for radial systems. 20
Instead, parameters are determined by measuring the impact body (transmitter) movement and the resulting force transmitted to the tissue phantom. The transmission tip and drive pressure used (for example, D = 20 mm, p = 4 bar) directly affect the results. 8
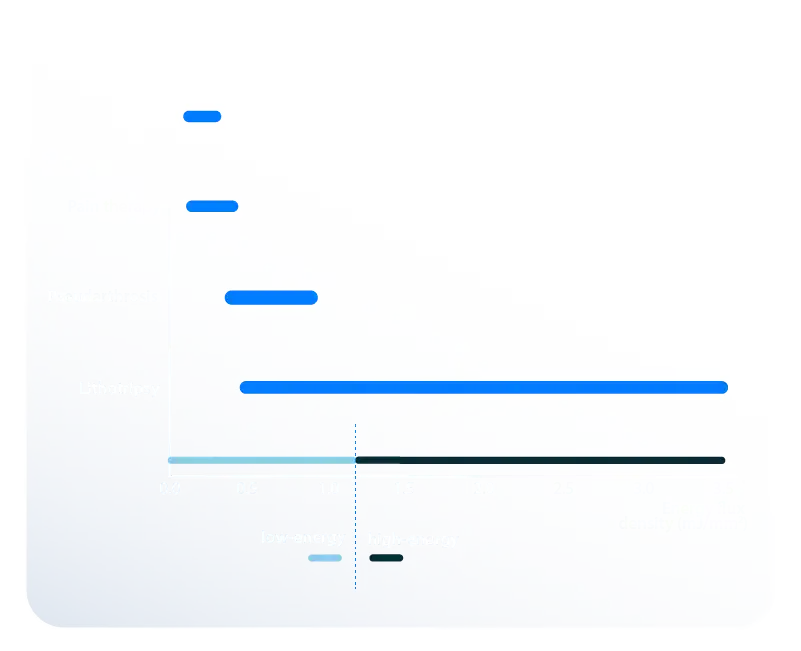
Shockwaves and pressure waves differ in terms of their formation mechanism, physical parameters, and therapeutic effect depths:
| Parameter | Shockwaves (Focused) |
Pressure Waves (Radial) |
| Pressure | 10 – 100 MPa | 0.1 – 1 MPa |
| Pulse Duration | ≈ 0.2 µs | ≈ 0.2 – 5 ms |
| Momentum | 0.5 – 2 mNs | 100 – 200 mNs |
| Energy | 20 – 35 mJ | 150 – 200 mJ |
| Pressure Gradient | 100 – 150 MPa/mm | 0.1 – 0.5 kPa/mm |
| Pressure Field | Focused | Radial, divergent |
| Penetration Depth | Large, up to 200 mm | Small, superficial, up to 50 mm |
| Affected Area | Cells | Superficial tissue |
Clinical Commentary
• Focused shockwaves are used for treating deep tissues and chronic trigger points.
• Radial pressure waves, on the other hand, are more effective for superficial soft tissue disorders.
• When both technologies are used together, treatment efficacy can be increased by targeting both superficial and deep tissues.